Overview
For the 2026–27 Federal Budget, ACRRM proposes three priorities to support a sustainable rural generalist workforce and improve access to high-quality healthcare for rural, remote and First Nations communities. These priorities are aimed at strengthening training pathways, supporting retention, and ensuring long-term workforce viability across rural Australia.
Budget Priority 1
ACRRM Calls for
- approval to provide 500 training places annually through the Australian General Practice Training (AGPT) program.
ACRRM supports the Australian Government’s delivery of the Strengthening Medicare: more bulk billing, more doctors and more nurses package which will see fully funded General Practitioner and Rural Generalist training places increase by an additional 300 places in 2027 and 400 places from 2028 in addition to the 1,500 commencing places currently offered through the AGPT program.
To assure continued growth of the Rural Generalist pipeline, ACRRM is seeking Australian Government approval under this commitment to deliver an additional 180 training places, taking the annual number of ACRRM training places to 500.
The only medical college dedicated to rural, remote and First Nations health, ACRRM has the capacity to take on these additional training places and deliver the quality training required to meet Australia’s rural and remote healthcare needs through a single integrated Rural Generalist Fellowship Program. For the 2026 training year, applications for ACRRM training places have increased by 30% and will be over subscribed for the third consecutive year, delivering on the current Australian Government contract by 115%. ACRRM has the demand, the experience and training model to sustainably deliver the additional training places sought in this proposal from 2027.
Funding for additional places has already been committed by the Australian Government1 in the 2025-26 Federal Budget. A decision of Government is required to dedicate the additional 180 places to ACRRM for the forward years, and an allocation under this previous Budget measure of $36 million a year over ACRRM’s 4-year Fellowship program.
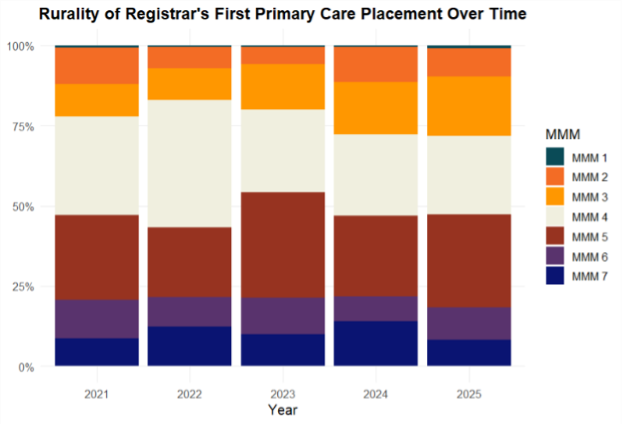
As shown in the table below, the large majority of ACRRM’s first registrar placements are in Modified Monash Model (MMM) areas 4-7, and more than 82% of FACRRMs are shown to still be working in rural communities five or more years after graduation.
By these measures, increasing the number of training places delivered by ACRRM will see an increase of specialist rural General Practitioners and Rural Generalists who will choose rural and remote careers and provide long-term healthcare much needed by these communities.
The rural and remote health workforce shortage persists throughout Australia, negatively impacting both the ability for people in these areas to access necessary services and their health outcomes. Dedicated government funding for fit-for-purpose workforce models, such as through the ACRRM Rural Generalist Fellowship Program is critical to improving service availability and the health of rural, remote, and First Nations communities.
Recognising the higher proportion of First Nations people in rural and remote areas, their health needs and importance of a First Nations medical workforce to deliver these services, ACRRM maintains a strong focus on increasing enrolments of First Nations registrars. First Nations registrars have a higher rate of returning to practise in their communities after Fellowship, as such, increasing representation will not only increase overall numbers in the workforce, but also increase rural and remote workforce specifically.
ACRRM remains committed to First Nations communities, with the College already meeting the Aboriginal and Torres Strait Islander performance indicator in the AGPT grant. The College has 4.35% of Aboriginal registrars in the Rural Generalist Fellowship programs. ACRRM will continue working with the Australian Government, partners and stakeholders to promote and identify opportunities for further investment in rural generalism and general practice as a potential career pathway for Aboriginal and Torres Strait Islander students.
References:
Budget Priority 2
ACRRM Calls for
- Rural Generalist access to relevant Medicare Benefit Scheme (MBS) item numbers
- Secure and strengthen rural maternity services.
As part of preparing the health system for formal recognition of Rural Generalist Medicine, appropriate recognition of the services provided by Rural Generalists within the MBS is critical to embedding the role within the Australian healthcare system and to recognising the value of Rural Generalists’ advanced skills in particular. This initiative seeks Rural Generalist MBS item numbers and/or service descriptors to facilitate access to an appropriate level of patient rebate2, as identified in the Rural Generalist recognition within the context of MBS item eligibility paper submitted to the Department of Health, Disability and Ageing (the Department) in April 2025 and summarised below:
- The establishment of 10 Rural Generalist-specific MBS items and two MBS telehealth items for when a Rural Generalist is providing patient care in their area of advanced skill;
- Access for Rural Generalists to 17 MBS items related to providing emergency care;
- 13 additional MBS items limited to Rural Generalists with advanced skill in mental health.
The principle underpinning this proposal has been recognised since the Australian Government, particularly through the National Rural Health Commissioner, commenced work on the National Rural Generalist Training Pathway:“ In relation to the MBS… Rural Generalists should have access to General Practice item numbers when providing General Practice services and access to relevant specialist item numbers when using their Additional Skills...including access to telehealth items.”3
This proposal also follows the established precedent of Rural Generalist obstetricians, anaesthetists and surgeons being able to claim relevant MBS items for services in the same way as their consultant specialist colleagues for equivalent services. It better aligns the MBS recognition with the full scope of practice of Rural Generalist practice, including core skills in primary care and emergency medicine, as well as individual areas of College-recognised advanced skills. These advanced skills span 13 disciplines and are formally recognised through ACRRM and/ or the RACGP.
As noted in the 2025 RDAA paper, ‘The MBS is the core of government funding for all outpatient services and therefore it is essential Rural Generalist Medicine is recognised within the MBS.’ The addition of these Rural Generalist MBS items will improve the affordability and availability of specialised health services in rural communities. This is particularly important given research that demonstrates a deficit in government spending on healthcare, pharmaceuticals, aged care and disability services of $967 less per person, per year in rural areas as compared to those in metropolitan areas. This includes a funding deficit of almost $400 per person per year through the MBS in very remote areas as compared to metropolitan areas4.
Further, by appropriately recognising and remunerating Rural Generalists through access to relevant MBS items, sustainability can be ensured for essential medical care to be delivered to rural, remote, and First Nations communities that need it most.
- Secure and strengthen rural maternity services
ACRRM supports and is a signatory to the National Consensus Framework for Rural Maternity Services (second edition) and seeks a clear commitment from the Australian Government to the principles of the Framework, including ongoing support and sustainable funding for rural maternity services. This commitment must include action to prevent further maternity service closures, targeted assistance to re-open services, and provision to support the viability of local birthing services.
Access to maternity services is increasingly difficult in rural and remote areas, as noted in the Framework: “Maternity services are not routinely provided in all rural hospitals and the downward trend of closures or intermittent periods of bypass in existing rural maternity facilities is continuing to occur across the country. When birthing services are closed and health professionals with maternity skills leave the community, risks for pregnant rural and remote women increase. As a result, women and families may have to travel significant distances for appointments and deliveries or relocate to a town or city with birthing facilities well before the birth is due. This comes with increased financial, social, cultural, and emotional costs for women and their families…Rural and remote women, like all women, want to be close to home during their pregnancies”. Rural Generalists and primary care teams must be adequately trained and supported, and services sustainably funded to ensure that safe, affordable and timely care close to home can be a reality for more women in rural Australia.
References:
2There is a geographical limitation for accessing the proposed rural generalist MBS items, to Modified Monash Model 3-7 locations
3 National Rural Generalist Taskforce Advice December 2018
4 The Forgotten Health Spend: A Report on the Expenditure Deficit in Rural Australia
5 Answering the Call for Regional Housing, 2025
6 Childcare deserts and oases: How accessible is childcare in Australia (2022)
Budget Priority 3
ACRRM Calls for
- Accessible and secure housing
- Quality childcare and early education services.
Supporting the professional and practicing environment of Rural Generalists is only one part of the recruitment and long-term retention story. It is critical to strengthen social infrastructure and foster strong rural communities to support Rural Generalists and their families. Targeted investments, recognition within relevant Australian Government initiatives and reforms for essential community services and social infrastructure are required to support rural and remote healthcare professionals as they care for their communities, including:
- Secure and accessible housing
- Childcare and early education
- Climate change action and disaster recovery support.
Secure and accessible housing
The availability of appropriate and secure housing is often a challenge in rural communities. The Regional Australia Institute (RAI) has found that ‘regional housing approvals are 20% lower than the early 2000s and failing to keep pace with population growth. House prices are growing faster in the regions in the cities”. Indeed, RAI identifies that “Australia’s rental crisis is, in face, a regional rental crisis – when it comes to securing a rental property, availability in the regions is consistently tighter and rent increases consistently faster than in capital cities’5.
The availability of appropriate housing options is necessary to ensure Rural Generalists can train, live and stay in their communities. Without somewhere to live that is safe and affordable, rural communities will not attract medical professionals or be seen as a long-term option for practitioners and their families. This must be recognised and addressed in housing initiatives and reforms of the Australian Government (for example, the National Housing Accord), to prioritise areas and projects where there are critical shortages of Rural Generalists in rural and remote Australia.
Childcare and early education
In addition to housing shortages, access to quality childcare and education is critical to support Rural Generalists and their families. While the Australian Government has legislated a three-day childcare guarantee - meaning that from January 2026, all eligible families will be guaranteed access to three days of subsidised childcare per week - the reality is that many rural and remote communities do not have the workforce and services available to deliver this guarantee, or meet the needs and hours often required of Rural Generalists and their families. In 2022, mapping of childcare access by Victoria University showed that 71.2% neighbourhoods designated as ‘childcare deserts’ were in rural and remote areas6.
It is critical that in programs, initiatives and reforms to enhance and improve access to childcare and early education services, the Australian Government recognises and prioritises areas of need for Rural Generalists and their families.
Climate change action and disaster recovery support
Climate Change has a flow-on impact on human health, and is increasingly shaping health system responses to natural disasters. ACRRM advocates for ongoing acknowledgement and awareness of the health impacts of climate change and calls on the Australian Government to adequately fund climate change action consistent with Net Zero ambitions and relevant to the rural and remote context, alongside the health system responses required and long-term support for natural disaster recovery support in affected rural and remote communities.
Submission documents and links:
Submission: ACRRM Pre-Budget Submission 2026 - 27
Media Releases:
For more information, please contact the policy team at policy@acrrm.org.au or 1800 223 226

